Orthostatic intolerance (OI) is one of the more common Long Covid symptoms (see this study). Othostatic intolerance is defined as a development of symptoms brought about by standing which resolve when sitting or lying down. Typically people with OI can become dizzy, lightheaded, have a rapid heart beat, heart palpitations, blurred vision, sweating and other problems when they stand up. They may even faint.
Normally, the autonomic nervous system is able to adjust the body’s systems when a person stands up. Standing sends thoracic (chest and abdomen) blood downward and away from the brain; the body automatically accounts for this through changes in blood pressure and heart rate, maintaining cerebral blood flow. Unfortunately people with orthostatic intolerance have a problem with this mechanism. Standing causes blood to drain downwards and compensation doesn’t occur, hence the dizziness, thumping heart and tendency to faint.
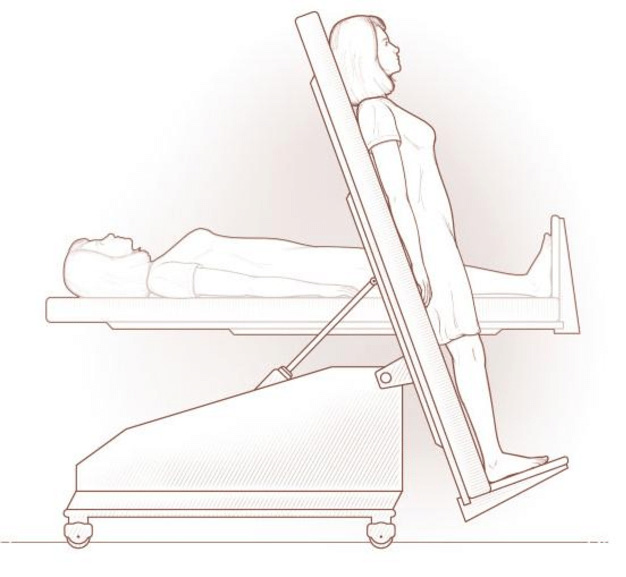
Orthostatic intolerance can be transitory or it can become a chronic condition. When combined with extreme changes in heart rate it is known as postural orthostatic tachycardia syndrome (POTS). To be officially diagnosed with POTS the body must have an increased heart rate of 30 beats per minute within ten minutes of standing up, while accompanied by symptoms. This increase should happen without a major drop in blood pressure (orthostatic hypotension). POTS is diagnosed by a cardiologist or specialist via a tilt table test. This is a special test where the patient is strapped to a horizontal table that can be mechanically tilted upright. Blood pressure and heart rate readings occur over a period of time, along with observation of symptoms.
Statistics are indicating the people with Long Covid commonly experience orthostatic intolerance. It’s not currently known whether this OI is a transient problem or is long term. A 2022 study suggested that while people with Long Covid may have OI, POTS was infrequent.
Advertisement
The Geek’s Guide To Long Covid is available as an ebook!
You’ll find a comprehensive guide to using wearables, apps and technology to cope with Long Covid. It offers detailed instructions on pacing, heart rate monitoring, HRV, POTS, deep breathing, tVNS, air purifiers, CO2 monitors and lots more.
Available from Amazon
How To Prove Orthostatic Intolerance or POTS to Your Doctor Via A Lean Test
POTS is a diagnosis requires a tilt table test. You need a referral for this to occur. If you are experiencing some of the symptoms of OI but they are transitory, it can be difficult to stress the need for a test to your doctor. Especially if you are only seeing them for a short amount of time in the usual appointment. There is a way to do this at home so that you can record your own results and present them to your doctor. (Note: Only do this if your OI doesn’t cause extreme symptoms like fainting).
It’s call a Lean Test. Sometimes the “NASA Lean Test”, because its a variant of the test NASA used on astronauts to test orthostatic intolerance after being weightless. The test is advocated by Lucinda Bateman MD, a researcher into ME/CFS and Fibromyalgia.

Ideally you need a second person to help you perform the test, however you may be able to do it alone if you have the right wearables (and aren’t likely to faint).
You’ll need a pulse oximeter and a blood pressure monitor/cuff. You can buy these at chemists (drugstores). Alternatively or additionally, you can use a Polar H10 chest strap and Heart Graph app. Have a timer handy.
It’s best to test a couple of hours after eating. Morning is a good time. You should stop taking any drugs used for OI (e.g. fludrocortisone), and limit water and salt intake for 24 hours. Do not wear compression socks or other compression clothing on the day of the test.
To do the test:
First, lie down for ten minutes. When you first lie down, and at the five minute and ten minute mark, have your friend take blood pressure and pulse readings. Write these numbers down.
After the ten minutes is up, lean up against a nearby wall with only your shoulder blades touching the wall. Your feet should be 15cm (6in) out from the wall. Try not to adjust your weight or move and limit talking. Your friend starts the timer and takes blood pressure and pulse readings at the start and then every minute for the next ten minutes.
Pay attention to your symptoms while standing and tell your friend to note them if they’re extreme, along with the time they occurred.
Your friend needs to watch you to make sure you don’t faint.
At the end of the 10 minutes you can lie down and rest. You may wish to record your BP and pulse after a couple of minutes, though it’s not strictly required.
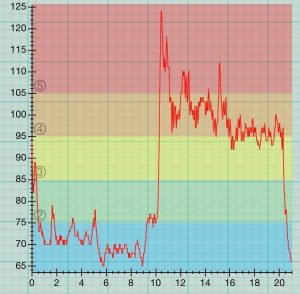
If you do the test with the Polar H10 and Heart Graph, you will only have a record of your heart rate. However, Heart Graph will give you a full record of your pulse over the 20 minutes and it will give a good idea of any major spikes or dips in your heart rate. Ideally, do the test with the BP monitor, pulse oximeter and chest strap/app combination. More info on Heart Graph here.
Here is Dr David S. Bell’s list of normal and abnormal results taking during OI tests:
- Normal Systolic BP: recumbent: 100-142; Standing (4 min): 94-141; Orthostatic change: -19 to +11
- Normal Diastolic BP: recumbent: 55-90; Standing: 61-97; Orthostatic change: -9 to +22
- Normal Pulse: recumbent: 54-96; Standing: 62-108; Orthostatic change: -6 to +27
- Orthostatic systolic hypotension: fall in systolic blood pressure of 20 mmHg or more
- Orthostatic diastolic hypotension: fall in diastolic BP of 10 mm Hg or more.
- Orthostatic diastolic hypertension: rise in diastolic BP to 98 mm Hg or higher
- Orthostatic narrowing of pulse pressure: reduction in pulse pressure to 18 mm Hg or lower.
- Orthostatic postural tachycardia: increase in heart rate of 28 bpm or to greater than 110 b/min.
Once you have your test results and a screenshot of Heart Graph, you can show them to your doctor and ask for further investigation. They may conduct a “standing test” in their office but be aware that you will not be as relaxed as at home so the results may show as more “normal”. This is where the Heart Graph option comes into its own because any major spikes are immediately apparent. Don’t be afraid to stand your ground, as it were, and ask for a tilt table test.
Treatment for POTS and Orthostatic Intolerance

Unfortunately, OI, POTS and autonomic dysfunction are considered to be difficult to treat. There is no current cure for POTS. Existing treatment consists of a mixture of medications, behavioural changes and, in some cases, exercise.
The main drug used to treat OI and POTS is Floudrocortisone (flourinef). It increases retention of salt and increases blood volume. This makes it easier for the heart to pump blood around the body. Side effects include headaches, water retention and high blood pressure. Other drugs include Erythropoietin, pyridostygmine (Mestinon) and medications that promote vasoconstriction – tightening of the veins. These include stimulants and some anti-depressants.
Mostly, OI and POTS are treated via behavioural modification. Patients are encouraged to take their time getting up, to avoid standing or prolonged sitting, and to avoid warm environments. Practically, this can mean:
- Using a shower chair or taking (relatively cool) baths
- Sitting down while cooking or doing other chores
- Ensuring the house has fans or air conditioning in summer.
- Eating smaller meals more often, as digestion can draw blood away from other areas and make OI worse.
- Using compression garments like thigh-high compression socks or girdles helps prevent the pooling of blood in the lower extremities.
- Increasing salt and water intake to encourage fluid retention. This means drinking 2-3 litres of water a day and taking salt tablets or 10-12 grams salt, the equivalent of 2-3 teaspoons of salt daily. This amount of salt is well over the maximum recommended amount for normal people. If you have hypertension, you should speak to your doctor about whether this is a good idea.
Exercise is also considered to be beneficial to POTS patients as it helps muscles to contract and send blood back to the brain. Because standing is difficult, exercises are typically performed in recumbent positions and may also include use of a recumbent bike. Cardiologist Benjamine Levine created his own exercise regime known as the Levine Protocol (or CHOPS/Dallas Modifed Program). This is based on his 2015 research that found people with POTS had improvements of symptoms after increased physical activity. You can find the Levine Protocol exercises in a pdf here.
Unfortunately, if you also have post exertional malaise or fatigue this complicates things. It may be difficult to accommodate the recommendations and they need to be adjusted. Or it may not be possible at all. You will need to talk to your doctor about this.
POTS Long Covid Recovery Stories
Stellate Ganglion Block: A January 2022 paper (Liu et.al.) reports that 2 patients had substantial recovery from Long Covid symptoms after being given a stellate ganglion block. This procedure involves injecting local anaesthetic into the stellate ganglion nerves in your neck. These nerves are part of the sympathetic nervous system that regulates unconscious bodily functions like heart rate and blood pressure. They also trigger immune system response. Stellate ganglion blocks are usually used to diagnose and treat circulation problems or nerve injuries. This time, however, the anesthetic was used to temporarily “turn off” the nerves and recalibrate the whole system back to balance. Both patients reported significant improvement in symptoms, some immediately and most within 60 days. The researchers said the procedure is very safe, has been used for over a century in other applications and is worth investigating as a treatment. A similar study was done on fibromyalgia patients in 1988 with promising results. Health Rising has an article on the study and the comments include another person who was helped by the therapy, plus suggestions of doctors who may do it. (https://www.healthrising.org/blog/2021/12/28/stellate-ganglion-long-covid-fibromyalgia/)
EECP: A September 2021 case report of a Long Covid Patient who had improvement in POTS symptoms after Enhanced External Counterpulsation (EECP) therapy. This therapy uses pressure on the lower limbs to increase blood flow. It’s a non-invasive outpatient therapy usually given to angina patients. The Long Covid patient was given 15 one hour treatments and reported improvement in brain fog, fatigue and her ability to walk to perform general daily activities. This is only a single person case study and the authors say it warrants further investigation.
Research
Raj, S.R., Arnold, A.C., Barboi, A. et al. Long-COVID postural tachycardia syndrome: an American Autonomic Society statement. Clin Auton Res 31, 365–368 (2021). https://doi.org/10.1007/s10286-021-00798-2
Monaghan A, Jennings G, Xue F, Byrne L, Duggan E and Romero-Ortuno R (2022) Orthostatic Intolerance in Adults Reporting Long COVID Symptoms Was Not Associated With Postural Orthostatic Tachycardia Syndrome. Front. Physiol. 13:833650. doi: 10.3389/fphys.2022.833650
Liu LD, Duricka DL. Stellate ganglion block reduces symptoms of Long COVID: A case series. J Neuroimmunol. 2022 Jan 15;362:577784. doi: 10.1016/j.jneuroim.2021.577784. Epub 2021 Dec 8. PMID: 34922127; PMCID: PMC8653406.
Bengtsson A, Bengtsson M. Regional sympathetic blockade in primary fibromyalgia. Pain. 1988 May;33(2):161-167. doi: 10.1016/0304-3959(88)90086-3. PMID: 3380557.
Varanasi S, Sathyamoorthy M, Chamakura S, Shah SA. Management of Long-COVID Postural Orthostatic Tachycardia Syndrome With Enhanced External Counterpulsation. Cureus. 2021 Sep 30;13(9):e18398. doi: 10.7759/cureus.18398. PMID: 34729276; PMCID: PMC8555928.
Links
10 Salty Facts for POTS Patients
POTS – Johns Hopkins Medicine
The Levine Protocol For Exercising With POTS