How to define Long Covid? In broad terms, it could be described as an illness caused by Covid-19 that lingers past the “acute” phase, which is technically two weeks, though some extend that to six weeks.
The World Health Organization names Long Covid as “Post COVID-19 Condition” and defines it thus:
“Post COVID-19 condition occurs in individuals with a history of probable or confirmed SARS CoV-2 infection, usually 3 months from the onset of COVID-19 with symptoms and that last for at least 2 months and cannot be explained by an alternative diagnosis. Common symptoms include fatigue, shortness of breath, cognitive dysfunction but also others and generally have an impact on everyday functioning. Symptoms may be new onset following initial recovery from an acute COVID-19 episode or persist from the initial illness. Symptoms may also fluctuate or relapse over time.”
– World Health Organisation, December 2021
Statistics vary but the WHO says 10-20% of people experience mid- to long-term effects after being infected with Covid-19. The length of time varies from weeks to months. Some people have had Long Covid for several years and have not recovered. Long Covid can occur after a relatively mild case of Covid 19. Severity of the acute illness has no bearing on the development of Long Covid. Symptoms can also appear weeks after a person has apparently recovered from the infection. People with Long Covid are sometimes described as “long haulers.” Other terms for Long Covid are “post-acute COVID-19 syndrome” and “post-acute sequelae of COVID-19 (PASC).”
Advertisement
The Geek’s Guide To Long Covid is available as an ebook!
You’ll find a comprehensive guide to using wearables, apps and technology to cope with Long Covid. It offers detailed instructions on pacing, heart rate monitoring, HRV, POTS, deep breathing, tVNS, air purifiers, CO2 monitors and lots more.
Available from Amazon
Risk factors for Long Covid include “female sex, belonging to an ethnic minority, socioeconomic deprivation, smoking, obesity and a wide range of comorbidities.”
Long Covid Symptoms
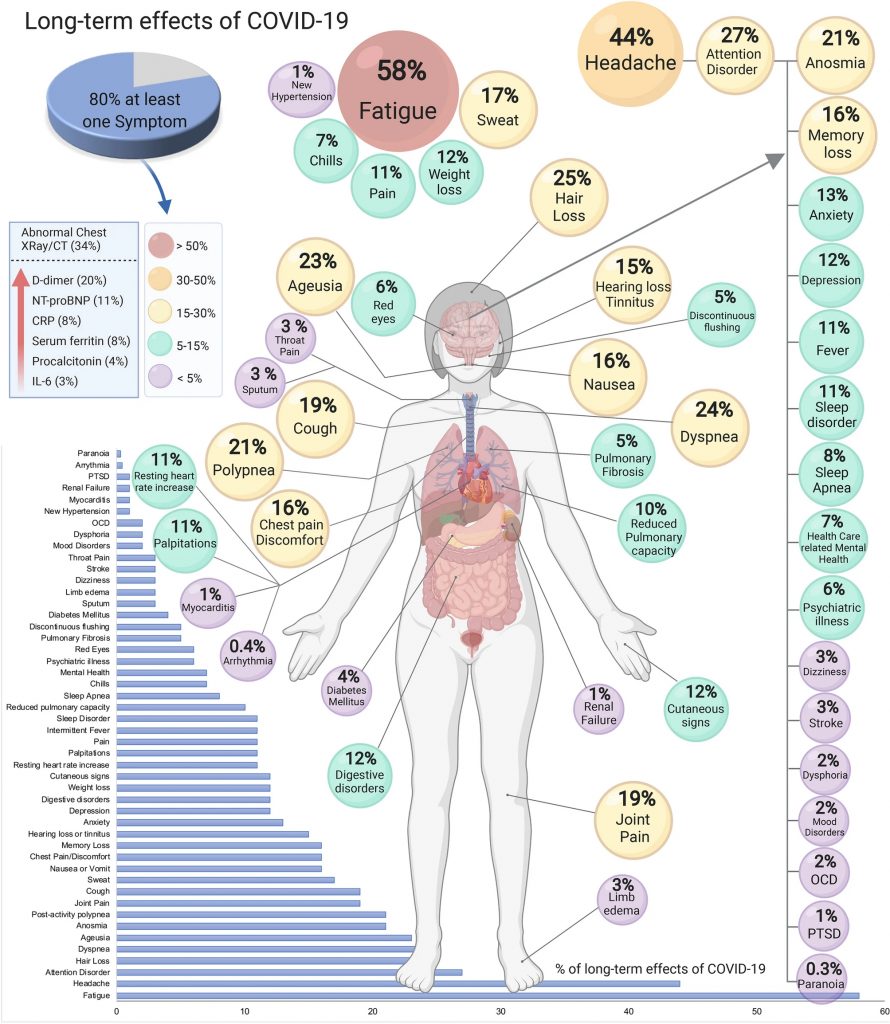
Long Covid presents as a wide variety of symptoms. These can be respiratory, circulatory and neurological or cognitive. A 2022 study of almost 500,000 people in the UK found a total of 62 symptoms were significantly associated with Covid. This expanded on a previous study where 55 long-term effects were identified.
- The most common symptoms are:
- Fatigue
- Shortness of breath
- Problems with sleep / insomnia
- Memory and concentration problems (brain fog)
- Loss of smell (anosmia) or taste
- Difficulty speaking
- Persistent cough
- Sneezing
- Chest pain, including lung/pleuristic pain and wider chest pain
- Muscle aches or joint pain
- Fever
- Depression or anxiety
- Hair loss
- Sexual dysfunction
- Other symptoms include:
- Orthostatic intolerance / Postural Orthostatic Tachycardia Syndrome (POTS)
- Skin rash
- Problems with the gut / diarrhoea
- Changes to vision
- Ear pain
- Phlegm
- Dry eyes
- Loss of periods / menorrhagia
- Hot flushes
- Dizziness / vertigo
- Issues with urine / urinary retention / Polyuria
Image: Long Term Effects of Covid 19
Long Covid Could Be Several Different Diseases.
Chahinda Ghossein, a physician and heart disease researcher at Maastricht University, is co-leading a large study of Long Covid patients in the Netherlands. She told Science.org: “The biggest obstacle that we are facing is we gave it one name, we gave it the name of Long Covid, which implies that it is one disease. All the studies being performed show us that it is not.”
The Subramanian 2022 study noted that there were three general types of Long Covid:
- General – Those with broad range of symptoms including fatigue, pain and headache, among many others. This comprised 80% of those studied
- Respiratory – Those whose symptoms were more focused on the respiratory system e.g. cough, shortness of breath, phlegm. This was 5.8% of those studied
- Cognitive / Mental Health – Those whose symptoms were more brain- or mentally-focused e.g. brain fog, insomnia, mental health problems, depression and anxiety.
A July 2022 preprint by the Zoe Health group found something very similar – grouping Long Covid patients by respiratory, neurological and general symptoms. A July 2022 preprint study found six distinct clusters of Long Covid patients. Acute illness severity and pre-existing conditions were often a predictor of what type of Long Covid people might have.
Long Covid may look different depending on the severity of the acute illness. Those who were hospitalized or had a severe case may experience lingering symptoms as a result of direct damage sustained during the initial illness. Those who develop Long Covid after a mild case may have more symptoms associated with immune dysfunction or other system-wide disorders.
Long Term Health Implications Of Covid Infection
New research shows that infection with COVID-19 – even mild cases – can increase the risk of illness and complications later in life. These include;
- Increased risk of blood clots and stroke (thromboembolic events) (Source)
- Increased risk of diabetes (Source)
- Increased risk of major cardiovascular events (Source)
- Increased risk of Alzheimers or dementia (Source)
- Increased or ongoing loss of memory or congnitive decline (Source) , especially in those who lost sense of smell during Covid (Source). One study found cognitive problems may be caused by lack of oxygen to the brain. The Yang study found inflammation and impaired circuitry in the brains of deceased Covid patients.
A 2021 study of hospitalized Covid patients in England found a third were re-admitted to hospital for various reasons within the first few months of being discharged. They had an increased risk of mortality and multiorgan dysfunction, including diabetes, cardiovascular events, liver or kidney disease.
What Causes Long Covid?
At this stage we still don’t know what causes Long Covid. Research has followed a number of differing theories as to the cause. These include:
Viral Persistence
Many viruses use RNA (ribonucleic acid) as their genetic blueprint. It’s the part of the virus that is injected into host cells so the virus can reproduce and spread. Researchers hypothesize that RNA fragments/proteins of the SARS-Cov2 virus, including the spike protein, persist in the lungs, gut, brain and other organs, long after the acute infection has passed. Another idea is that the virus may persist in a hidden “reservoir” within the body.
The existence of viral fragments may stimulate an ongoing immune reaction, causing inflammation and multi-system dysfunction. Several pre-print studies have found evidence for this (Chertow et al. 2021, Swank et al, 2022), with fragments persisting up to 230 days after infection.
A May 2022 study found people with Long Covid had more than 100 times more Covid-specific T-cells than people who had recovered from the virus. They hypothesized that the high levels of T-cells indicate ongoing infection in hidden reservoirs. The theory is unproven as yet but researchers are hoping that viral persistence may provide a biomarker for Long Covid in the future. The study suggested antivirals like Paxlovid may be a possible treatment.
Micro Clots
Red blood cells transport oxygen to the muscles, brain and other cells throughout the body. A clot is a thickened cluster of red blood cells designed to stop bleeding during an injury. When blood clots form inside veins it has the potential to move and cause heart attacks or strokes. A “microclot” or microembolism is a relatively recent discovery.
South African researchers found that Covid causes persistent tiny clots of the red blood cells, both in acute and Long Covid cases (Grobbelaar et al. 2021, Pretorius et al. 2021). Normally the body breaks down microclots via a process called fibrinolysis but this process may not occur in Long Covid patients. The researchers believe inflammatory molecules become trapped in the microclots. The clots impede blood flow and cause more clotting. The result is less oxygen getting to the body’s cells and an ongoing state of inflammation. This results in shortness of breath, brain fog and ongoing malaise. The clots can also damage or kill small nerve fibres, resulting in dysautonomia. A related theory posits that the lining of the blood vessels have been damaged and thus less oxygen is reaching the cells. The theory is unproven but more research is being done.
Immune System Dysfunction
The immune system is our body’s natural defence mechanism. When infected with a pathogen like a virus or bacteria, the immune system reacts to kill the invader, remove damaged body cells and prepare for any future attack. It does this with a variety of white blood cells that work together to find, identify, remove and remember the invader.
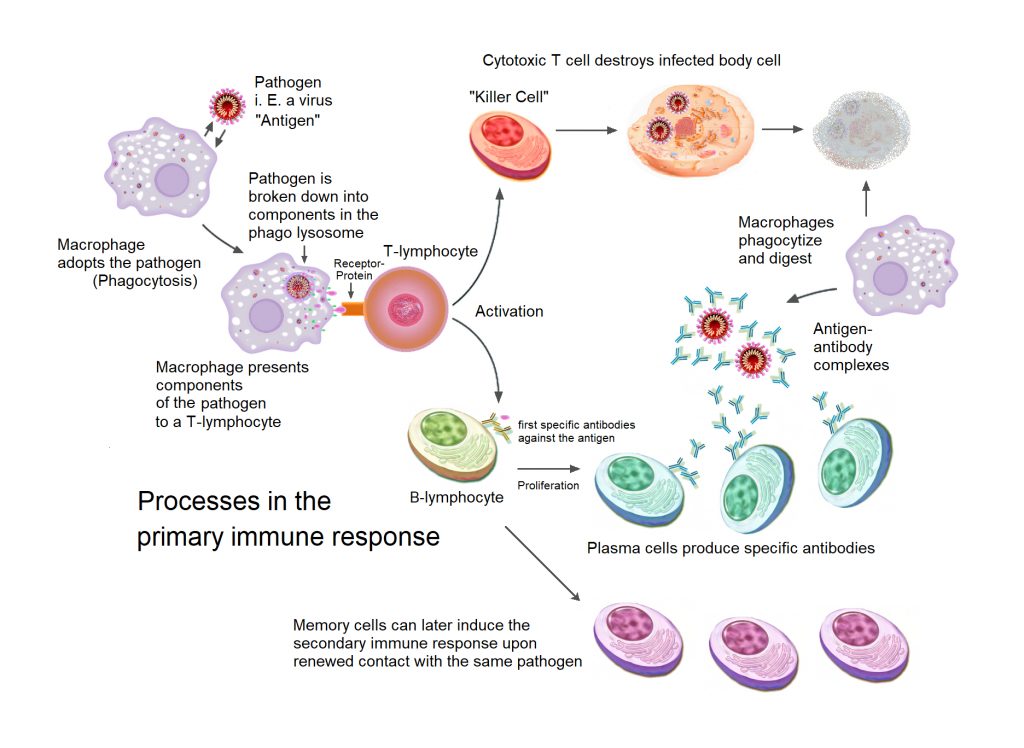
In theory, the immune system is so destabilized by Covid that it stays on “high alert” and is unable to reset itself. Research published in January 2022 found that Long Covid patients had immunological dysfunction persisting for 8 months after infection. They found that white blood cells were extremely active, especially T- and B-cells, signaling chronic inflammation.
A different 2022 study offered the contradictory suggestion that the immune system may actually be suppressed in some Long Covid patients. A March 2022 study found that autoantibodies – immune system proteins that attack or affect the body rather than the invading pathogen – were prevalent in those suffering acute COVID-19 and then persisted for months in Long Covid patients. This suggests Long Covid could be an auto-immune problem. Another study found immune dysfunction resulted in small-fibre neuropathy (nerve damage) and this may account for symptoms such as orthostatic intolerance, gut problems, autonomic dysfunction, shoulder pain and tingling sensations in the skin. More research needs to be done.
Gut Microbiome Changes
The gut microbiome is the bacteria, fungus and other flora that live in the human intestine. We’re only just starting to learn how the gut biome affects our health but research shows it can play a part in obesity, mental health and immune function.
A 2022 Hong Kong study found people with Long Covid had a less diverse gut biome six months after their illness compared to people who hadn’t had Covid. An earlier study of a smaller group had similar results. Dr David Strain, Chair of BMA Board of Science and Clinical senior lecturer and honorary consultant. University of Exeter Medical School, said: “This finding is consistent with several existing hypotheses that Long Covid may be associated with a small quantity of residual virus in the immuno-privileged tissue (i.e the regions of the body such as the gut, that the protection of our antibodies doesn’t reach). It also accounts for the observations that we have seen non-genetically related households (e.g. husband and wife) affected by long COVID more than would be anticipated.”
Reactivation of Dormant Viruses
The Epstein-Barr Virus (EBV) is a type of herpes virus that causes glandular fever. The virus is so common that around 95% of people have been infected in their lifetime. The virus remains in the body after infection and replicates at a low level in our mouths and noses but usually doesn’t cause further symptoms. This is known as a latent or dormant infection.
A large 2022 study suggests that a reactivation of latent EBV may be causing at least some cases of Long Covid. The study looked at post severe-acute Long Covid patients and found high levels of auto-antibodies, which suggested an autoimmune response. They found that one third of patients had reactivated EBV infections and suggested it may play a role in Long Covid symptoms. They also found that the patient’s immune systems had ramped up before they got Covid, suggesting a predisposition to ongoing illness. A June 2021 study also found that two thirds of Long Covid patients had EBV reactivation.
Renin-Angiotensin System Dysfunction
The Renin-Angiotensin System (RAS) is a group of related hormones that regulate your blood pressure. Renin is an enzyme that is created by the kidneys. It works with the cardiovascular system to control blood volume (how much blood you have) and vascular pressure (the relaxation and constriction of your blood vessels. It also plays a part in the immune system, renal system and the gut microbiome. The SARS-CoV-2 virus spreads with the help of the RAS system and thus causes disruption to the whole system, possibly in the long term. This disruption would account for ongoing inflammation / immune problems, orthostatic intolerance and heart problems and lack of oxygen due to circulatory problems (exhaustion and brain fog).
Pick Your Dysfunction
Beyond these theories as to what could be causing Long Covid, there’s a wider body of research into multi-system dysfunction and how it all interacts to create chronic disease. ME/CFS researchers have taken a variety of approaches when studying that disease and, given the similarities with Long Covid, you may hear about these issues at some point.
Autonomic Nervous System Dysfunction
The autonomic nervous system is the part of your body that regulates unconscious mechanisms like breathing, heart rate, blood pressure, digestion and the function of internal organs. These things help keep you alive and the ANS operates without you having to think about it. The ANS has two main modes or systems:
Sympathetic – the “fight or flight” mode. This response exists to protect us from threats and can be seen as a stress response. It speeds up the heart, dilates the pupils, slows digestion and can put bodily functions “on hold” until the threat is over.
Parasympathetic – the “rest and digest” mode. This bodily response kicks in when you are resting or not stressed. It slows the heart rate, encourages food to be digested and enables repair and recovery from illness.
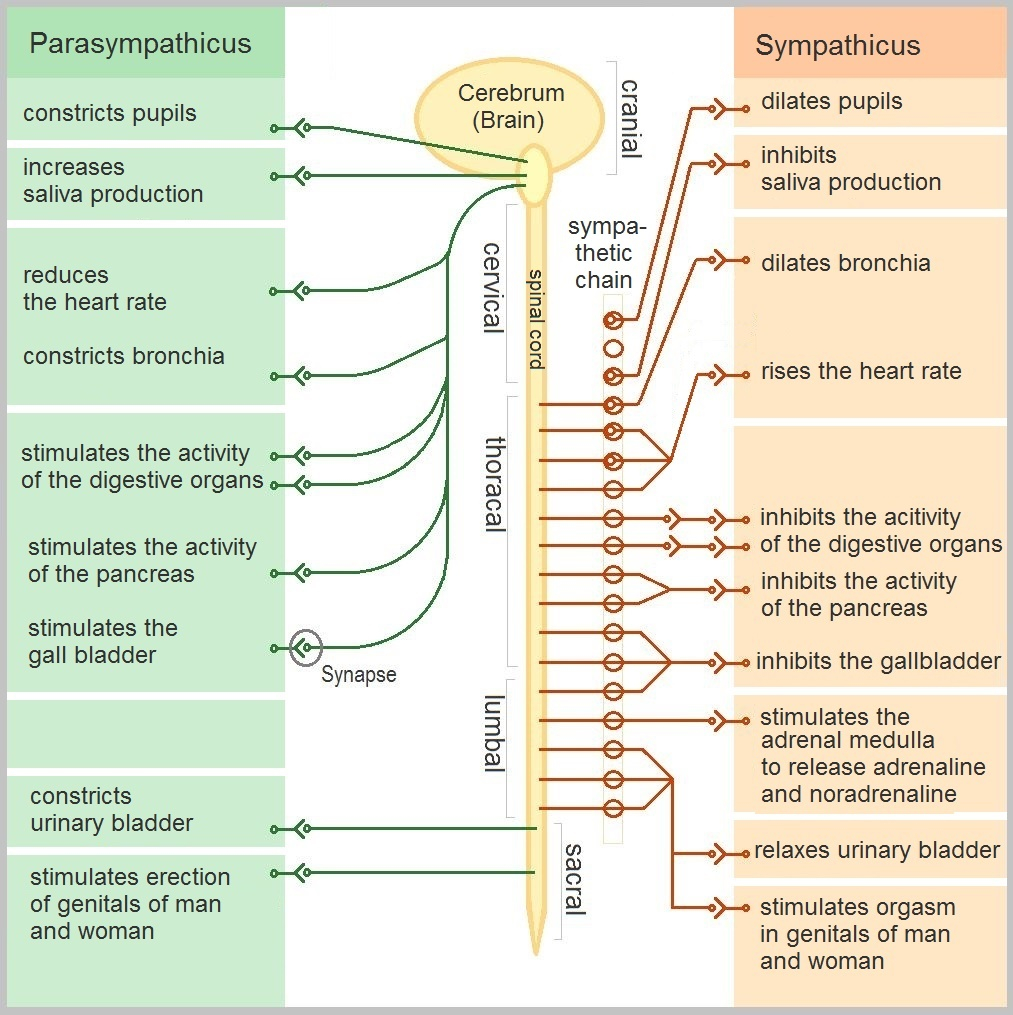
When the body is functioning well, these two modes operate in balance with each other. Illness and stress can cause the pendulum to swing too far in one direction, either sympathetic or parasympathetic, and dysautonomia is the medical term for when the ANS does not function properly. Dysautonomia symptoms include orthostatic intolerance, heart rate changes (bradycardia and tachycardia), palpitations, blood pressure changes and parathesia, among many others. Dysautonomia seems to be a common aspect of Long Covid. A 2022 preprint study found 67% of Long Covid patients had moderate to severe autonomic dysfunction.
You’ll find more information on Dysautonomia on the HRV page.
Mast Cell Activation Disorders
Mast cells are a type of white blood cells commonly found in parts of the body that interact with the outside environment found in the skin, like the intestinal lining, cardiac and respiratory systems and the neural system, among others. Mast cells are like a first line of defence. When they encounter a pathogen or allergen, they release chemicals into the blood and lymph system that sets off the body’s immune system. Mast Cell Activation Disorders occur when mast cells are overactive; either there’s too many of them or the existing ones misfire and release immune system chemicals without an allergen to trigger it. The latter is known as Mast Cell Activation Syndrome (MCAS). Overactivity of mast cells can result in unnecessary allergic reactions and symptoms like itching, hives, runny nose, trouble breathing, headache, rapid heart rate and other problems. The response can range from mild to life-threatening. Mast cell disorders have no cure but are treated with antihistamines and corticosteroids.
Mast cells are what incites the “cytokyne storm” intense immune reaction to COVID-19. A 2021 study found mast cell activation symptoms were very common in Long Covid patients.
Mitochondrial Dysfunction, Lactate and Oxidative Stress
The mitochondria is the “power plant of the cell”. It’s where our cells turn food into energy – more specifically, converting glucose and oxygen into a chemical called ATP, which our cells need to function. Mitochondria have their own DNA that if damaged, can cause fairly serious illnesses.
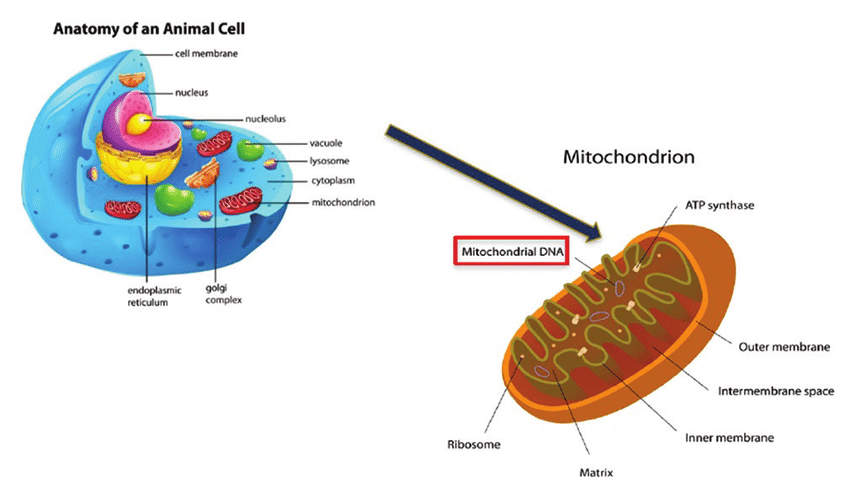
There is a theory that people with ME/CFS and maybe Long Covid have some kind of mitochondrial dysfunction or damage (Wood et al. 2021). Their cells have difficulty generating enough ATP, resulting in low energy and ongoing fatigue, especially after exercise. A 2022 study also found that people with Long Covid have decreased fatty acid oxidation and altered lactate production. Lactate (or lactic acid) is a byproduct of ATP production that can cause muscle pain and fatigue. Fatty acids are part of what the mitochondria break down to make energy.
Mitochondria can also make energy without oxygen (known as glycolysis or anaerobic production), however this doesn’t produce as much energy. It also creates more lactic acid. This process typically occurs when a person exercises intensely but it can’t be maintained for long. Researchers have hypothesized that people with ME/CFS reach the anerobic threshold at lower levels of activity than healthy people and this results in post-exertional fatigue. It’s possible that Long Covid patients experience the same process. There is a hypothesis that the COVID-19 virus causes the mitochondria to switch to anaerobic production in order to speed the replication of more virus. This would result in ongoing mitochondrial dysfunction.
Oxidative stress occurs when there is an imbalance of free radicals and antioxidants in the body. Free radicals are the byproduct of oxygen reactions and they cause damage to mitochondria, which means the mitochondria don’t work or aren’t able to replace themselves. Usually the body produces antioxidants which neutralise free radicals and balance is maintained. Diet, lifestyle, pollution and illness can cause an excess of free radicals. A 2022 study found COVID-19 patients had increased levels of oxidative stress and oxidant damage, and low levels of glutathione, an antioxidant. That study suggested supplementation with glutathione, though no trials have been done on this as yet.
At time of writing, researchers in the UK are conducting a clinical trial into mitochondrial enhancer drug called AXA1125. The study was due for completion July 2022. See more info on the Treatment page.
Heart, Vascular and Breathing Dysfunction
Cells need oxygen to make energy and our circulatory system delivers oxygen from our lungs to our cells. It’s possible that the oxygen isn’t being delivered as efficiently in people with Long Covid and that explains the fatigue, shortness of breath and inability to exercise that many people experience. One 2022 study looked at whether oxygen was being diffused through the smallest blood vessels in Long Covid patients. It found that those who had severe disease often had lost many of those vessels, leading to lack of oxygen in the blood. Mild patients retained the small vessels but oxygen wasn’t being diffused through them, though it was getting through larger vessels. Even so, there was still less oxygen in the blood.
Harvard pulmonologist Dr. David Systrom is looking at exercise intolerance in both Long Covid and ME/CFS patients. His latest study found patients who had recovered from COVID-19 had markedly reduced oxygen use during exercise and their blood vessels had impaired oxygen extraction. The study also found inefficiency with ventilation in these patients – their breathing provided less oxygen.
The same researchers have found that people with ME/CFS often have “preload failure”. This is when the large veins in the legs and abdomen don’t push enough blood up to the right side of the heart. They proposed that small fiber neuropathy may be causing problems with blood vessels, resulting in blood not reaching muscles or the heart due the veins not constricting properly. It’s possible the same process occurs in Long Covid.
Long Covid and ME/CFS patients often describe “air hunger” – a feeling of not getting enough oxygen. A 2021 study of ME/CFS patients found a large number of them exhibit hypcapnia, which is abnormally low levels of carbon dioxide (CO2) in the blood, due to hyperventilation (overbreathing). Another 2022 study found ME/CFS patients were breathing slower and more deeply because their bodies were trying to adjust to less oxygen reaching the muscles.
It’s also possible that the heart is not speeding up as it should during exertion. This is called chronotropic incompetence and is can be a symptom of autonomic nervous system dysfunction (see above). Subsets of people with Long Covid have been shown to have chronotropic incompetence and researchers suggest it be tested for and treated.
HPA Axis and Cortisol (?)
The HPA Axis describes the complex feedback system between the hypothalamus, pituitary gland, and adrenal glands. Hormones produced by these glands regulate stress reactions, our immune system and fertility. The main hormone associated with the HPA axis is cortisol, the “stress hormone”. Cortisol is activated when we need to protect ourselves from danger. Together with adrenaline, it’s the hormonal aspect of the “fight or flight” response. Among other things, cortisol suppresses antibody production and stimulates pro-inflammatory T-cell death. When we’re stressed, cortisol levels remain high and this can eventually cause damage to tissues and health problems. When the adrenal glands produce too little cortisol, this is called Addison’s disease. When there’s too much cortisol, it’s called Cushing’s Syndrome.
Unfortunately, the HPA axis hasn’t been studied extensively as yet so there’s a lot we don’t understand. There also hasn’t been much research into Covid and cortisol or the HPA axis. A single study of 28 people found that the adrenocortical response was impaired in people with COVID-19 and that they had low cortisol levels consistent with adrenal insufficiency. It’s possible that HPA axis dysfunction could explain Long Covid but a lot more research needs to be done.
Be aware: Alternative medicine often mentions “adrenal fatigue”. To date, the existence of this illness is unproven. Studies attempting to investigate it have produced conflicting results and the methodology has been questioned (Ross, 2018; Cadegiani et al. 2016).
What We Do Know About Long Covid
While scientists uncover more about Long Covid, there are some things we do know about Long Covid. One is that it is definitely a real phenomenon and that millions of people are now suffering because of it. We also know that the world is currently experiencing a mass-disabling event due to Long Covid and governments need to take it seriously. We know that people with Long Covid deserve better support, especially since so many governments have taken a “let it rip and forget it” approach to Covid.
Find out more about Long Covid treatment options here.
Note: Sex and gender exist on a spectrum. On this site the terms “male” and “female” refer to sex assigned at birth.
References
Subramanian, A., Nirantharakumar, K., Hughes, S. et al. Symptoms and risk factors for long COVID in non-hospitalized adults. Nat Med (2022). https://doi.org/10.1038/s41591-022-01909-w
Canas, Liane S, et al. Profiling post-COVID syndrome across different variants of SARS-CoV-2 (Preprint), 31 July 2022, medRxiv 2022.07.28.22278159; doi: https://doi.org/10.1101/2022.07.28.22278159
Reese J, et al; and the RECOVER Consortium. Generalizable Long COVID Subtypes: Findings from the NIH N3C and RECOVER Programs. medRxiv [Preprint]. 2022 May 25:2022.05.24.22275398. doi: 10.1101/2022.05.24.22275398. PMID: 35665012; PMCID: PMC9164456.
Lopez-Leon, S., Wegman-Ostrosky, T., Perelman, C. et al. More than 50 long-term effects of COVID-19: a systematic review and meta-analysis. Sci Rep 11, 16144 (2021). https://doi.org/10.1038/s41598-021-95565-8
Ho FK, Man KKC, Toshner M, Church C, Celis-Morales C, Wong ICK, Berry C, Sattar N, Pell JP. Thromboembolic Risk in Hospitalized and Nonhospitalized COVID-19 Patients: A Self-Controlled Case Series Analysis of a Nationwide Cohort. Mayo Clin Proc. 2021 Oct;96(10):2587-2597. doi: 10.1016/j.mayocp.2021.07.002. Epub 2021 Jul 16. PMID: 34607634; PMCID: PMC8282478.
PHOSP-COVID Collaborative Group. Clinical characteristics with inflammation profiling of long COVID and association with 1-year recovery following hospitalisation in the UK: a prospective observational study. Lancet Respir Med. 2022 Apr 22:S2213-2600(22)00127-8. doi: 10.1016/S2213-2600(22)00127-8. Epub ahead of print. PMID: 35472304; PMCID: PMC9034855.
Yang, A.C., Kern, F., Losada, P.M. et al. Dysregulation of brain and choroid plexus cell types in severe COVID-19. Nature 595, 565–571 (2021). https://doi.org/10.1038/s41586-021-03710-0
Søraas A, Bø R, Kalleberg KT, Støer NC, Ellingjord-Dale M, Landrø NI. Self-reported Memory Problems 8 Months After COVID-19 Infection. JAMA Netw Open. 2021;4(7):e2118717. doi:10.1001/jamanetworkopen.2021.18717
de Erausquin Gabriel A. et al. Olfactory dysfunction and chronic cognitive impairment following SARS-CoV-2 infection in a sample of older adults from the Andes mountains of Argentina. Presentation at 2021 Alzheimer’s Association International Conference July 2021
Ayoubkhani D, Khunti K, Nafilyan V, Maddox T, Humberstone B, Diamond I et al. Post-covid syndrome in individuals admitted to hospital with covid-19: retrospective cohort study BMJ 2021; 372 :n693 doi:10.1136/bmj.n693
Ramakrishnan RK, Kashour T, Hamid Q, Halwani R, Tleyjeh IM. Unraveling the Mystery Surrounding Post-Acute Sequelae of COVID-19. Front Immunol. 2021 Jun 30;12:686029. doi: 10.3389/fimmu.2021.686029. PMID: 34276671; PMCID: PMC8278217.
Chertow, D et al. SARS-CoV-2 infection and persistence throughout the human body and brain (preprint), December 2021, https://doi.org/10.21203/rs.3.rs-1139035/v1
Swank, Z. et al. Persistent circulating SARS-CoV-2 spike is associated with post-acute COVID-19 sequelae (preprint), June 2022, https://doi.org/10.1101/2022.06.14.22276401
Littlefield KM, Watson RO, Schneider JM, Neff CP, Yamada E, et al. (2022) SARS-CoV-2-specific T cells associate with inflammation and reduced lung function in pulmonary post-acute sequalae of SARS-CoV-2. PLOS Pathogens 18(5): e1010359. https://doi.org/10.1371/journal.ppat.1010359
Grobbelaar LM, Venter C, Vlok M, Ngoepe M, Laubscher GJ, Lourens PJ, Steenkamp J, Kell DB, Pretorius E. SARS-CoV-2 spike protein S1 induces fibrin(ogen) resistant to fibrinolysis: implications for microclot formation in COVID-19. Biosci Rep. 2021 Aug 27;41(8):BSR20210611. doi: 10.1042/BSR20210611. PMID: 34328172; PMCID: PMC8380922.
Pretorius, E., Vlok, M., Venter, C. et al. Persistent clotting protein pathology in Long COVID/Post-Acute Sequelae of COVID-19 (PASC) is accompanied by increased levels of antiplasmin. Cardiovasc Diabetol 20, 172 (2021). https://doi.org/10.1186/s12933-021-01359-7
Buonsenso D. et al., Evidence of lung perfusion defects and ongoing inflammation in an adolescent with post-acute sequelae of SARS-CoV-2 infection, Lancet Child Adolesc Health 2021;5: 677–80 Published Online, July 2021. https://doi.org/10.1016/S2352-4642(21)00196-6
Phetsouphanh, C., Darley, D.R., Wilson, D.B. et al. Immunological dysfunction persists for 8 months following initial mild-to-moderate SARS-CoV-2 infection. Nat Immunol 23, 210–216 (2022). https://doi.org/10.1038/s41590-021-01113-x
Gaylis, Norman B., Angela Ritter, Scott A Kelly, Nader Z Pourhassan, Meenakshi Tiwary, Jonah B Sacha, Scott G Hansen, Christopher Recknor, Otto O Yang, Reduced Cell Surface Levels of C-C Chemokine Receptor 5 and Immunosuppression in Long Coronavirus Disease 2019 Syndrome, Clinical Infectious Diseases, 2022;, ciac226,
Su et al. Multiple early factors anticipate post-acute COVID-19 sequelae, 2022, Cell 185, 881–895 DOI:https://doi.org/10.1016/j.cell.2022.01.014
Oaklander, Anne Louise, Alexander J. Mills, Mary Kelley, Lisa S. Toran, Bryan Smith, Marinos C. Dalakas, Avindra Nath, Peripheral Neuropathy Evaluations of Patients With Prolonged Long COVID, Neurol Neuroimmunol Neuroinflamm May 2022, 9 (3) e1146; DOI: 10.1212/NXI.0000000000001146
Liu Q, Mak JWY, Su Q, et al, Gut microbiota dynamics in a prospective cohort of patients with post-acute COVID-19 syndrome, Gut 2022;71:544-552.
Chen Y, Gu S, Chen Y, et al, Six-month follow-up of gut microbiota richness in patients with COVID-19, Gut 2022;71:222-225.
Gold JE, Okyay RA, Licht WE, Hurley DJ. Investigation of Long COVID Prevalence and Its Relationship to Epstein-Barr Virus Reactivation. Pathogens. 2021 Jun 17;10(6):763. doi: 10.3390/pathogens10060763. PMID: 34204243; PMCID: PMC8233978.
Larsen, Nicholas W., Lauren E. Stiles, Ruba Shaik, Logan Schneider, Srikanth Muppidi, Cheuk To Tsui, Mitchell G. Miglis. Characterization of Autonomic Symptom Burden in Long COVID: A Global Survey of 2,314 Adults, April 2022, medRxiv 2022.04.25.22274300; doi: https://doi.org/10.1101/2022.04.25.22274300
Khazaal, Shaymaa & Harb, Julien & Rima, Mohamad & Annweiler, Cédric & Wu, Yingliang & Cao, Zhijian & Khattar, Ziad & Legros, Christian & Kovacic, Hervé & Fajloun, Ziad & Sabatier, jean-marc. (2022). The Pathophysiology of Long COVID throughout the Renin-Angiotensin System. Molecules. 27. 2903. 10.3390/molecules27092903.
Weinstock LB, Brook JB, Walters AS, Goris A, Afrin LB, Molderings GJ. Mast cell activation symptoms are prevalent in Long-COVID. Int J Infect Dis. 2021 Nov;112:217-226. doi: 10.1016/j.ijid.2021.09.043. Epub 2021 Sep 23. PMID: 34563706; PMCID: PMC8459548.
Wood E, Hall KH, Tate W. Role of mitochondria, oxidative stress and the response to antioxidants in myalgic encephalomyelitis/chronic fatigue syndrome: A possible approach to SARS-CoV-2 ‘long-haulers’? Chronic Dis Transl Med. 2021 Mar;7(1):14-26. doi: 10.1016/j.cdtm.2020.11.002. Epub 2020 Nov 21. PMID: 33251031; PMCID: PMC7680046.
de Boer E, Petrache I, Goldstein NM, Olin JT, Keith RC, Modena B, Mohning MP, Yunt ZX, San-Millán I, Swigris JJ. Decreased Fatty Acid Oxidation and Altered Lactate Production during Exercise in Patients with Post-acute COVID-19 Syndrome. Am J Respir Crit Care Med. 2022 Jan 1;205(1):126-129. doi: 10.1164/rccm.202108-1903LE. PMID: 34665688; PMCID: PMC8865580.
Kumar, Premranjan , Ob Osahon, David B. Vides, Nicola Hanania, Charles G. Minard, Rajagopal V. Sekhar. Severe Glutathione Deficiency, Oxidative Stress and Oxidant Damage in Adults Hospitalized with COVID-19: Implications for GlyNAC (Glycine and N-Acetylcysteine) Supplementation. Antioxidants, 2021; 11 (1): 50 DOI: 10.3390/antiox11010050
Matheson AM, McIntosh MJ, Kooner HK, Lee J, Desaigoudar V, Bier E, Driehuys B, Svenningsen S, Santyr GE, Kirby M, Albert MS, Shepelytskyi Y, Grynko V, Ouriadov A, Abdelrazek M, Dhaliwal I, Nicholson JM, Parraga G. Persistent 129Xe MRI Pulmonary and CT Vascular Abnormalities in Symptomatic Individuals with Post-Acute COVID-19 Syndrome. Radiology. 2022 Jun 28:220492. doi: 10.1148/radiol.220492. Epub ahead of print. PMID: 35762891; PMCID: PMC9272782.
Singh I, Joseph P, Heerdt PM, Cullinan M, Lutchmansingh DD, Gulati M, Possick JD, Systrom DM, Waxman AB. Persistent Exertional Intolerance After COVID-19: Insights From Invasive Cardiopulmonary Exercise Testing. Chest. 2022 Jan;161(1):54-63. doi: 10.1016/j.chest.2021.08.010. Epub 2021 Aug 11. PMID: 34389297; PMCID: PMC8354807.
Joseph P, Arevalo C, Oliveira RKF, Faria-Urbina M, Felsenstein D, Oaklander AL, Systrom DM. Insights From Invasive Cardiopulmonary Exercise Testing of Patients With Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Chest. 2021 Aug;160(2):642-651. doi: 10.1016/j.chest.2021.01.082. Epub 2021 Feb 10. PMID: 33577778; PMCID: PMC8727854.
Natelson BH, Lin JS, Blate M, Khan S, Chen Y, Unger ER. Physiological assessment of orthostatic intolerance in chronic fatigue syndrome. J Transl Med. 2022 Feb 16;20(1):95. doi: 10.1186/s12967-022-03289-8. PMID: 35172863; PMCID: PMC8849016.
Cook DB, VanRiper S, Dougherty RJ, Lindheimer JB, Falvo MJ, Chen Y, Lin JS, Unger ER; MCAM Study Group. Cardiopulmonary, metabolic, and perceptual responses during exercise in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): A Multi-site Clinical Assessment of ME/CFS (MCAM) sub-study. PLoS One. 2022 Mar 15;17(3):e0265315. doi: 10.1371/journal.pone.0265315. PMID: 35290404; PMCID: PMC8923458
Jimeno-Almazán A, Pallarés JG, Buendía-Romero Á, Martínez-Cava A, Courel-Ibáñez J. Chronotropic Incompetence in Non-Hospitalized Patients with Post-COVID-19 Syndrome. J Clin Med. 2021 Nov 20;10(22):5434. doi: 10.3390/jcm10225434. PMID: 34830716; PMCID: PMC8617992.
Alzahrani AS, Mukhtar N, Aljomaiah A, Aljamei H, Bakhsh A, Alsudani N, Elsayed T, Alrashidi N, Fadel R, Alqahtani E, Raef H, Butt MI, Sulaiman O. The Impact of COVID-19 Viral Infection on the Hypothalamic-Pituitary-Adrenal Axis. Endocr Pract. 2021 Feb;27(2):83-89. doi: 10.1016/j.eprac.2020.10.014. Epub 2020 Dec 15. PMID: 33554871; PMCID: PMC7837186.
Ross IL, Jones J, Blockman M. We are tired of ‘adrenal fatigue’. S Afr Med J. 2018 Aug 28;108(9):724-725. doi: 10.7196/SAMJ.2018.v108i9.13292. PMID: 30182895
Cadegiani FA, Kater CE. Adrenal fatigue does not exist: a systematic review. BMC Endocr Disord. 2016 Aug 24;16(1):48. doi: 10.1186/s12902-016-0128-4. Erratum in: BMC Endocr Disord. 2016 Nov 16;16(1):63. PMID: 27557747; PMCID: PMC4997656.
Article last updated August 2022. Check the Long Covid News page to see if there’s new info.