There are currently no official treatment options for Long Covid. The disease is new, still being studied and has a large variety of symptoms. At present, doctors are treating symptoms individually.
Treating The Cause Of Long Covid
At present no-one knows the cause of Long Covid. There are, however, a number of overarching theories as to the root cause of it all (see What Is Long Covid?) and these lead to possible treatments using existing drugs. Here’s some hypothetical / unproven drug treatments.
Antivirals like Paxlovid
If the theory of viral persistence (hidden reservoirs of virus in the body) is true, antiviral drugs like Paxlovid (nirmatrelvir and ritonavir) may help. At present there’s only anecdotal evidence of people with Long Covid recovering some or all of their health after taking Paxlovid. Other long haulers have had no luck with it. A 2022 preprint of several case studies showed that the timing of the antiviral therapy affected the outcomes. In November 2022, Stanford University started a clinical trial, backed by Pfizer, to see if Paxlovid could reduce symptoms of Long Covid. The results are due in September 2023. Meanwhile, m clinical trials are needed.

There are a few other trials underway looking at other antivirals, including the Bateman Horne Center, looking at the combination of Valaciclovir and Celecoxib, however results are not out yet.
Advertisement
The Geek’s Guide To Long Covid is available as an ebook!
You’ll find a comprehensive guide to using wearables, apps and technology to cope with Long Covid. It offers detailed instructions on pacing, heart rate monitoring, HRV, POTS, deep breathing, tVNS, air purifiers, CO2 monitors and lots more.
Available from Amazon
Covid vaccine
Some people with Long Covid have reported improvement after receiving the COVID-19 vaccine or a booster. In theory the vaccine antibodies help clear lingering virus from hidden reservoirs.
A July 2022 study of 186 people with Long Covid found that there was no evidence that vaccination improved symptoms. Other evidence is mostly anecdotal. A Facebook poll found 13% of long haulers felt better after the vaccine. The BMJ reported on three small studies looking at the effect of vaccines on Long Covid patients. These studies did not find any conclusive evidence that the vaccine will help, though they had methodological issues. The were not able to pinpoint exactly how the vaccine might help long haulers.
Aspirin, blood thinners, anticoagulants and anti-platelet therapy
If Long Covid is caused by microclots in the blood preventing oxygen transport to the tissues then it makes sense to take a drug that will cause the clots to break up. The same South African researchers who found microclots in the blood have done a follow up study with a suggested treatment (currently the study is in preprint). They gave 24 patients Clopidogrel 75mg and Aspirin 75mg once a day, as well as a direct oral anticoagulant Apixiban 5 mg twice a day plus Pantoprazole 40 mg perday for gastric protection. All 24 said their main symptoms were resolved. Keep in mind this is a pre-print study not a clinical trial, there were no controls and it has not bee peer-reviewed yet.
The Stimulate-ICP group has just embarked on a large study of Long Covid patients, testing several drugs. One of these is Rivaroxaban, used to treat blood clots, specifically deep vein thrombosis and pulmonary embolism. Their site doesn’t specify dosages and says people should not try it outside of clinical trials.
It’s worth noting that the RECOVERY trial – a huge international project looking at treatments for COVID-19 – found that aspirin didn’t prevent people from dying but was associated with a small increase in people getting out of hospital earlier. The trial doesn’t look at Long Covid.
While aspirin is easily available and seems like a simple option to explore for Long Covid, it’s best to consult a doctor before using as it can cause bleeding, bruising and other issues.
Statins
Statins are drugs used to reduce cholesterol in people at risk of cardiovascular disease. Anyone who has had COVID-19 is at a higher risk of cardiovascular problems so statins may be prescribed as a preventative measure for some post-COVID-19 patients. Statins also have an anti-inflammatory effect. Initial studies suggested statins reduced the severity of COVID-19 but a more recent piece of research suggested this isn’t the case. A number of well known doctors like Dr Michael Mosley and Dr. Bruce Patterson have advocated the use of statins in treating Long Covid but there’s no published research on this as yet.
Antihistamines
Mast cell activation occurs in a large number of Long Covid patients resulting in allergy-like symptoms. Persistent inflammation is also an issue. In theory antihistamines such as Loratidine (Claratyne) or Fexofenadine may help. It’s worth noting that there are two types of antihistamine drugs, classified by the receptors they bind to in the body. H1 receptor antihistamines are an older form. H2 antihistamines don’t cause drowsiness and have a longer half life. Both types are being considered as treatments for mast cell disorders in Long Covid.

A 2021 observational study of Long Covid patients found 72% of patients had clinical improvement after treatment with histamine receptor antagonists. Over four weeks they were given a combination of H1 (Loratadine 10 mg two times per day or Fexofenadine 180 mg two times per day) and H2 (Famotidine 40 mg once daily or Nizatidine 300 mg once daily). Science Direct offers two case studies of antihistamine use on Long Covid patients here.
The Stimulate-ICP group is also studying a combination otf Loratidine and Famotidine, an antihistamine that works on the stomach and intestines but the results are not out yet. Beyond this there’s anecdotal evidence and several case reports to suggest antihistamines are helpful but not a lot of other studies. Even so, over-the-counter antihistamines are readily available and have few side effects so you may consider them worth pursuing. Again, talk to your doctor first.
Immune system drugs, mono-clonal antibodies and anti-inflammatory drugs
In theory the inflammation caused by acute COVID-19 infection can cause damage to the immune system, possible autoimmunity and ongoing inflammation. Drugs that downregulate the immune system or treat inflammation may help Long Covid patients. Antibodies are the body’s natural immune defence against viruses. Mono-clonal antibodies are artificial antibodies created to help kick off your immune response. Typically they’re used on acute cases of COVID-19.
Examples of possible immune / anti-inflammatory drugs:
– Corticosteroids are a class of drugs usually used to reduce inflammation. They mimic the effect of hormones like cortisol. An increase in these hormones suppress the immune system which can help dampen down inflammation. Corticosteroids can have nasty side effects and long-term use is not recommended. Treatment of acute COVID-19 typically involves some use of corticosteroids such as Dexamethsazone.
When it comes to Long Covid, there hasn’t been a lot of research, though anecdotally there a lot of people advocating for their use, especially Prednisone and Prednisolone. One study of four people found Prednisone improved symptoms. Corticosteroids may dampen the immune system but can also increase blood pressure and heart rate, potentially making some symptoms worse. Suppressing the immune system may also raise the risk of infection – including a re-infection with COVID-19. They can also interact with other drugs like aspirin. Discussion with a doctor is advised.
– Colchicine is a drug usually used to treat gout but it has become a subject of study for both acute and Long Covid. It’s an anti-inflammatory drug that has been used to treat inflammation of the lining of the heart (percarditis). It may help a subset of Long Covid patients with heart problems and may also provide a more broad anti-inflammatory effect across the entire body. A UK site offering clinical guidance to GPs offering care to Long Covid patients suggests Colchicine as an option if there are heart problems.
The Stimulate-ICP group is studying Colchicine as a possible treatment for Long Covid. The trial has only started so there are no results yet.
Colchicine was considered as a treatment for acute COVID-19 but the RECOVERY trial found it did not make much of a difference in preventing death or helping people recover earlier. This means that some doctors are discounting its use. The trial doesn’t look at Long Covid.
– Ampligen is a drug by AIM Immunotech with immunomodulatory and antiviral properties. It improves the function of natural killer (NK) cells, which are immune cells from the same family as T- and B- cells. The company is in phrase III of an initial pilot study looking at how Ampligen works on ME/CFS and Long Covid patients. An update from 29 July 2022 found patients had statistically significant improvements in chronic fatigue. The next stage is a proper controlled clinical trial.
– CCR5 Antagonists. CCR5 is a protein found on the surface of white blood cells. It’s a chemical receptor that helps the cell move to where it’s needed during infection. It acts as a receptor for cytokines – the inflammatory villain of COVID-19. Research has previous found that blocking the receptor helps fight HIV. In an out-of-balance immune system – which may be the cause of Long Covid – blocking CCR5 receptors may help. Some CCR5 antagonist drugs include Aplaviroc, Leronlimab, Vicriviroc and Maraviroc.
— Leronlimab. A 2022 study treated 55 Long Covid patients with either the mono-clonal antibody drug Leronlimab or a placebo. They found those who took Leronlimab showed an improvement in their symptoms. They also had an increase in immune cells. Dr Otto Yang from the research team told Medical News Today that “Patients who improved were those who started with low CCR5 on their T cells, suggesting their immune system was less active than normal, and levels of CCR5 actually increased in people who improved.” This suggests an under-active immune system – rather than over-active as many supposed – may be the cause of Long Covid.
Note: In February 2022 CytoDyn, the makers of Leronlimab were told by the US FDA to issue an official correction on their website pointing out that the drug has not been officially approved for any treatment. The FDA have also released an official statement about Leronlimab.
– Low Dose Naltrexone (LDN). Naltrexone is usually used to treat alcohol and drug addiction. It works by blocking opioid receptors in the brain. Beyond this official use, Naltrexone is now prescribed off-label in low doses for a variety of problems, including rheumatoid arthritis, MS and ME/CFS (read more at LDN Research Trust). It works in two ways. First, the low dose blocks the opioid receptors for only a short time and to compensate, the brain makes more endorphins, resulting in less pain and feeling of wellbeing. Secondly, it has an anti-inflammatory effect and helps the immune system.
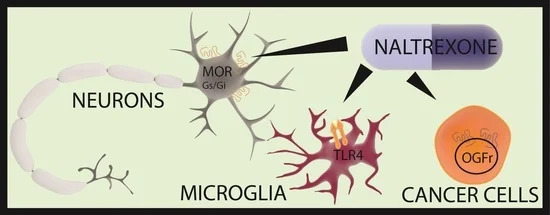
Researchers at Griffith University in Australia have found that LDN improves the functioning of natural killer (NK cells) and may benefit people with ME/CFS. A 2017 study found LDN reduced pro-inflammatory cytokines in people with Fibromyalgia. Research into whether LDN will work with Long Covid is underway including one combining LDN and Colchicine.
Because low dose Naltrexone is used experimentally off-label, you will need to talk to your doctor about its use. The low doses need to be compounded into a separate tablet. Alternatively you can dilute regular 50mg tablets in water and dose with pipette.
– IV Immunoglobulins. Immunoglobulins are another word for antibodies. People with autoimmune diseases are treated with immunoglobulin products which are made from donated blood plasma. These products usually contain immunoglobulin G (IgG) and small amounts of immunoglobulin A (IgA) – IgG is the key ingredient that helps to fight disease-causing substances, such as viruses and bacteria. The product in introduced intravenously so a transfusion of immunoglobulins is known as IVIG. Current COVID-19 guidelines don’t recommend the use of IVIG on acute cases. There’s also been very little research done on IVIG on Long Covid. A May 2022 study of 17 Long Covid patients found IVIG was helpful in relieving small fiber neuropathy. Beyond that, there’s not a lot of evidence for it. IVIG is expensive and difficult to obtain; the therapy is only approved for certain autoimmune conditions in many countries.
Mitochondrial Enhancers
If mitochondrial dysfunction is at the root of Long Covid, there’s not a lot of existing drugs available to treat it. A clinical trial by Oxford University and Axcella Therapeutics is underway. This trial is testing a proprietary amino acid compound called AXA1125 on Long Covid patients. The components as listed in an earlier study are: Leucine – 1.00 gram, Isoleucine: 0.50 gram, Valine: 0.50 gram, Arginine: 1.81 grams, Glutamine: 2.00 grams, N-Acetyl-Cysteine: 0.15 gram.
The company claims this compound increases fatty acid oxidation, improves anti-oxidant response, restores cellular energy and reduces inflammation. Whether their claims are true will of course depend on the trial results.
Treating The Symptoms Of Long Covid

Official treatment guidelines for Long Covid are typically sparse, given there’s so much we don’t know about the disease. Guidelines tend to emphasise rest and pacing activity to conserve energy. Respiratory therapy and breathing exercises are suggested for shortness of breath. Cognitive therapy may help for brain fog, speech and memory problems. Some guidelines suggest graded exercise and cognitive behavioural therapy, a combination that used to be commonly recommended for people with ME/CFS but is now discredited and not used for that illness. Graded exercise may work for some but not all Long Covid patients.
Ideally, treatment for the symptoms of Long Covid should be tailored to each individual depending on their circumstances.
Heart and Respiratory Problems
Anyone who has had COVID-19 is at a higher risk of cardiovascular problems including heart attack, stroke, myocarditis, pericarditis, dysrhythmias and a bunch of other issues (read the study here). This means being vigilant about chest pain and any symptoms involving the chest, heartbeat and circulation. Tests such as chest x-rays, CT scans, echocardiograms and respiratory tests may identify issues that are relatively easy to treat.
Myocarditis (inflammation of the heart muscle) and pericarditis (inflammation of the lining of the heart) usually resolve on their own. These problems are treated with rest and sometimes corticosteroids, intravenous immunoglobulin or medication for heart failure.
Heart and respiratory symptoms like palpitations, tachycardia/bradycardia, shortness of breath and blood pressure problems may be related to dysautonomia (see below).
Fatigue
Chronic fatigue doesn’t have one single treatment. Usually dealing with it involves a mixture of rest, lifestyle changes and occasionally drugs or supplements.
Resting becomes very important. This means ensuring you get enough sleep and keep good sleep hygiene. This mean getting enough hours of sleep, avoiding screens before bed, sleeping in a quiet dark room and keeping a regular bedtime. Regular rest breaks during the day can help, whether they be meditation, sitting down or naps.
Pacing is one way of coping with ongoing fatigue. It’s the process of finding a baseline of activity that doesn’t induce excess fatigue. It means adapting your life and activities to suit a lower amount of available energy. A 2021 online survey conducted by the Patient-Led Research Collaborative found that many participants found pacing to be “significantly helpful” in recovery. See Pacing page for a lot more detail.

Image by Eliza Lake from Pixabay
Heart rate monitoring is one way to keep track of daily exertion and maintain a steady level of energy. See the Heart rate monitoring page for a lot more detail.
Medication for fatigue is a hit-and-miss affair. Anti-depressants such as Wellbutrin or selective serotonin reuptake inhibitors may be an option for some but won’t work for others. Sleeping tablets may provide some relief from insomnia but they don’t encourage deep sleep which is vital for ongoing recovery.
A number of supplements and alternative medications claim to reduce fatigue. As with most supplements and vitamins, there isn’t a lot of evidence to back up their claims. One exception might be CoQ10. Co-Enzyme Q10 (Ubiquinone/ubiquinol) is an antioxidant that can also enhance ATP (energy) production in the mitochondria. A 2021 study found that combining CoQ10 with NADH, another coenzyme, resulted in better sleep and less fatigue in people with ME/CFS. Ubiquinol is the more easily absorbed form of CoQ10. Side effects are minimal but it may cause insomnia in some.
It’s worth having a thyroid function test to ensure you are not deficient in vitamin B12. If your levels are on the low side, consider supplementing vitamin B12.
Dysautonomia
Dysfunction of the autonomic nervous system is common in Long Covid patients. Dysautonomia symptoms include orthostatic intolerance (see below), heart rate changes (bradycardia and tachycardia), palpitations, blood pressure changes and parathesia, among many others.
Treatment for dysautonomia is hit and miss because the disease is not well understood. SSRI and tricyclic anti-depressants may help some. Experimental treatments involve stimulating the vagus nerve, the longest nerve in the autonomic system. This nerve can excite a parasympathetic response from the autonomic nervous system, calming symptoms. Vagus nerve stimulation exercises include deep breathing, humming, certain yoga poses and cold water. Electrical stimulation of the nerve with a TENS machines (tVNS) is an experimental practice. Read more on the HRV / Dysautonomia page or the tVNS page.
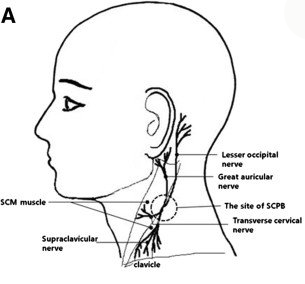
– Stellate Ganglion Block (SGB) An experimental treatment called Stellate Ganglion Block (SGB) has been said to help some Long Covid patients with dysautonomia. The stellate ganglion nerve is a group of neuron cells that run down the sides of the neck. These nerves as strongly associated with the sympathetic nervous system. SGB involves temporarily blocking these nerve signals with local anaesthetic. It’s usually used to treat head, neck and chest pain but experimentally it’s being used as a treatment for PTSD, anxiety and depression.
Now researchers are proposing SGB as a treatment for dysautonomia in Long Covid patients. The idea is that the block will give the autonomic nervous system a chance to reset and thus calm down chronic the sympathetic “fight or flight” response.
A January 2022 case study saw two Long Covid patients successfully treated with SGB. An April 2022 Newsweek article quoted David Gaskin, a Texas nurse anesthetist, who said he’d performed an SGB on over 200 patients with a 85-90% success rate. Not a lot of other research has occurred so this treatment remains very experimental (and also rather expensive).
POTS and Orthostatic Intolerance
A large number of Long Covid patients are experiencing orthostatic intolerance or Postural Orthostatic Tachycardia Syndrome (POTS). This is when your blood pressure doesn’t adapt to standing and can result in heart rate spikes, dizziness and fainting spells. Treatment for POTS involves increasing salt intake, compression garments and a reclining exercise regime. See the Orthostatic Intolerance page for a lot more detail.
Drug treatments for POTS are mainly experimental. These include Floudrocortisone (Flourinef) and Desmopressin, which encourage fluid retention and a subsequent increase in blood volume, and Clonidine, which is usually used to control high blood pressure. Midodrine and Ocreotide cause the blood vessels in the legs to constrict, keeping blood flowing back to the heart and brain. Beta blockers and calcium channel blockers are another option. More info here.
Recently researchers have been looking at the off-label use of Ivabradine, which is usually prescribed for heart failure. It is a selective funny channel blocker (yes, funny channels are a thing in the heart) that works by slowing down the heart rate. A February 2021 study of people with hyperadrenergic POTS found that ivabradine significantly improved heart rate and quality of life.
Neuropathy
A subset of Long Covid patients experience tingling in the hands and feet. Small fiber neuropathy is nerve damage caused by COVID-19. Thankfully, small nerve fibers can heal themselves with time. Corticosteroids or intravenous immunoglobulin have been successfully used to treat small fiber neuropathy in Long Covid patients.
Allergy / Histamine Response
Large numbers of Long Covid patients have mast cell problems resulting in allergy-like symptoms. As mentioned above, over-the-counter antihistamines may assist in relieving symptoms like sneezing, hives, runny nose and itching. A doctor may be able to advise on the best type of antihistamine to take for your particular problem.
Some Long Covid support groups recommend a low-histamine diet. This involves avoiding tinned, fermented and pickled foods, cured or processed meats, fruits and vegies like oranges and tomatoes, wine and beer and some nuts. It also involves avoiding leftovers or food that has been stored for a length of time. Identifying histamine intolerance involves cutting a lot of things out of your diet and adding them back over time.
The Association of UK Dietitians advises against undertaking a low histamine diet because there’s no evidence that it works for Long Covid. Cutting certain foods out of your diet may cause nutritional deficits and, importantly, take away a source of joy.
Gut and Digestive Problems
A subset of Long Covid patients experience ongoing problems with their digestive system including abdominal pain, constipation, diarrhoea, nausea and vomiting. It’s possible that the virus has caused inflammation of the gut lining or disrupted the gut biome. It may also be possible that autoantibodies are attacking the gut causing problems.
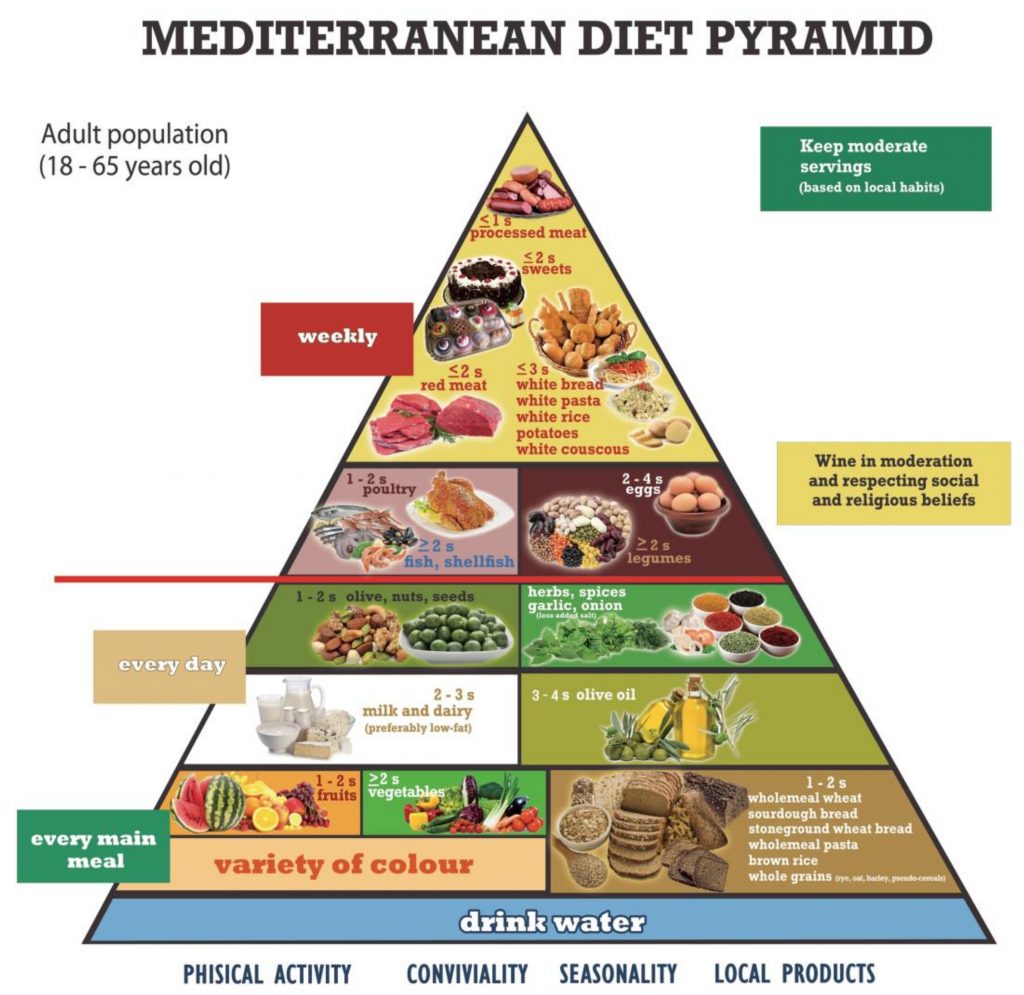
Diet is important in improving and maintaining gut health. Unsurprisingly a lot of fad diets have popped up claiming to help with Long Covid. The official Association of UK Dietitians recommends eating a healthy Mediterranean-style diet that is high in fibre and plant-based foods (see image below). They do not recommend restrictive diets or taking lots as vitamins as there is no evidence this helps. They do recommend taking Vitamin D if you are unable to get out into the sunshine. Avoiding unnecessary antibiotics will also maintain gut health.
– Probiotics. It’s possible to heal a disrupted gut biome (where unhealthy bacteria and other flora outnumber the good ones) by eating more prebiotic and probiotic foods. Prebiotics are food sources that encourage the growth of good bacteria in your gut. These are usually fruit, vegetables and legumes like chickpeas and lentils. Soluble and insoluble fibre sources also help. The best sources of probiotics are fermented foods with live cultures like sauerkraut, kimchi, some yoghurts, miso and kombucha (more info here and here).
The two recognised forms of good bacteria are the Lactobacillus species and the Bifidobacterium species. You can buy supplements containing these good bacteria but there’s not a lot of evidence that they help. There are three main issues with supplements. One is how many live bacteria are actually in the pill. Some may not survive on the shelf. The second is the dosage – how many probiotic bacteria are needed to treat an individual may vary. The third issue is whether any probiotic can survive the stomach acid and make it into the intestines. Lactobacillus and Bifidobacterium are the best candidates for surviving the trip. Supplement capsules with an enteric (protective) coating are the most likely to work.
A 2021 UK study found Long Covid patients who took a priobiotics mix of 5 species of lactobacillus with inulin made from chicory had significant improvement in their symptoms over 30 days (more info here). Inulin is a fermentable fiber that bacteria feed on, which encourages the growth of good bacteria. The researchers, called the Phyto-V group, also looked at whether a capsule rich in plant chemicals could be added to the probiotics and improve outcomes.
– Fecal Transplants. Fecal transplants for Long Covid are being investigated as a possible treatment. A fecal transplant is a way of introducing good gut flora into an unhealthy gut using a stool (poop) sample from a healthy person. They are usually delivered via colonoscopy. This is a surgical procedure where a tube with a camera is inserted into the intestine via the anus. The donated fecal sample is mixed with water and is sprayed into the intestine. A gastroscopy, where the tube goes down the throat, is an alternative. Both require sedation. It’s also possible to receive a fecal transplant via an enteric-coated pill but this is relatively new. Fecal transplants are mainly used when people have an infection of Clostridium difficile bacteria.
At present there’s not a lot of evidence that a fecal transplant will help Long Covid. Some early preliminary case studies describe fecal transplants rapidly resolving acute COVID-19 infections. Beyond that, no studies have been done.
Loss of Smell and Taste
In some people SARS-COV-2 virus invades the olfactory nerves and damage the sense of smell or taste. Some people with Long Covid have not recovered these senses, or had only partial recovery. At present, the main consensus treatment recommended by olfactory experts is smell training. This involves sniffing strong smelling substances and identifying them. In theory this retrains the brain’s sense of smell. Experts suggest this is a better option that treatment with corticosteroids.
A small clinical trial by Thomas Jefferson University Hospital tested the use of platelet-rich plasma (PRP) on Long Covid patients. PRP is a common treatment used to regenerate cells. It’s created from a patient’s own blood plasma and may help stem cells to regenerate nerves. Researchers applied PRP to a sponge and placed it high in the nose, once a month for three months. The small study only had 8 participants. Half of them showed improvement of their taste and smell. A 2020 pilot study of 7 people injected the PRP into the nose. It showed the procedure was safe and possibly effective. More research is needed.
Links
Guidelines summary of Recommendations for the recognition, diagnosis, and management of long COVID (UK Clinical Guidelines Summary Site)
Long Covid: what we know about it and how best to treat it (The Guardian, 10 July 2022)
Some Patients Are Reporting Long COVID Recoveries—But Experts Still Don’t Fully Understand Why (Time, 9 June 2021)
Drugmakers, scientists begin the hunt for long COVID treatments (Reuters, 25 March 2022)
Existing Drugs May Be Capable of Helping COVID Long-Haulers Recover (VeryWellHealth, 5 July 2021)
References
Peluso, Michael J., Khamal Anglin, Matthew S. Durstenfeld et al. Effect of oral nirmatrelvir on Long COVID symptoms: a case series, 05 May 2022, PREPRINT (Version 2) available at Research Square https://doi.org/10.21203/rs.3.rs-1617822/v2
Wynberg E, Han AX, Boyd A, van Willigen HDG, Verveen A, Lebbink R, van der Straten K, Kootstra N, van Gils MJ, Russell C, Leenstra T, de Jong MD, de Bree GJ, Prins M; RECoVERED Study Group. The effect of SARS-CoV-2 vaccination on post-acute sequelae of COVID-19 (PASC): A prospective cohort study. Vaccine. 2022 Jul 30;40(32):4424-4431. doi: 10.1016/j.vaccine.2022.05.090. Epub 2022 Jun 7. PMID: 35725782; PMCID: PMC9170535.
Sivan M, Greenhalgh T, Milne R, Delaney B. Are vaccines a potential treatment for long covid? BMJ 2022; 377 :o988 doi:10.1136/bmj.o988
Pretorius, Etheresia, et al. Combined triple treatment of fibrin amyloid microclots and platelet pathology in individuals with Long COVID/ Post-Acute Sequelae of COVID-19 (PASC) can resolve their persistent symptoms (PREPRINT), May 2022, Research Square. https://doi.org/10.21203/rs.3.rs-1205453/v2
RECOVERY Collaborative Group, Aspirin in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial, November 17, 2021, The Lancet. DOI:https://doi.org/10.1016/S0140-6736
Wu KS, Lin PC, Chen YS, Pan TC, Tang PL. The use of statins was associated with reduced COVID-19 mortality: a systematic review and meta-analysis. Ann Med. 2021 Dec;53(1):874-884. doi: 10.1080/07853890.2021.1933165. PMID: 34096808; PMCID: PMC8189130.
Bikdeli, Behnood, et al, Atorvastatin Versus Placebo In Critically-ill Patients With Covid-19: The Inspiration-S Double Blind Randomized Controlled Trial, https://www.abstractsonline.com/pp8/#!/9228/presentation/24055. https://www.everydayhealth.com/coronavirus/statins-do-not-improve-covid-19-outcomes-study-shows/
Glynne P, Tahmasebi N, Gant V, et al, Long COVID following mild SARS-CoV-2 infection: characteristic T cell alterations and response to antihistamines, Journal of Investigative Medicine 2022;70:61-67. October 2021
Utrero-Rico A, Ruiz-Ruigómez M, Laguna-Goya R, Arrieta-Ortubay E, Chivite-Lacaba M, González-Cuadrado C, Lalueza A, Almendro-Vazquez P, Serrano A, Aguado JM, Lumbreras C, Paz-Artal E. A Short Corticosteroid Course Reduces Symptoms and Immunological Alterations Underlying Long-COVID. Biomedicines. 2021 Oct 26;9(11):1540. doi: 10.3390/biomedicines9111540. PMID: 34829769; PMCID: PMC8614904.
RECOVERY Collaborative Group, Colchicine in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial, October 2021, The Lancet, DOI:https://doi.org/10.1016/S2213-2600(21)00435-5
Gaylis, Norman B., Angela Ritter, Scott A Kelly, Nader Z Pourhassan, Meenakshi Tiwary, Jonah B Sacha, Scott G Hansen, Christopher Recknor, Otto O Yang, Reduced Cell Surface Levels of C-C Chemokine Receptor 5 and Immunosuppression in Long Coronavirus Disease 2019 Syndrome, Clinical Infectious Diseases, 2022;, ciac226, https://doi.org/10.1093/cid/ciac226
Cabanas H, Muraki K, Staines D, Marshall-Gradisnik S. Naltrexone Restores Impaired Transient Receptor Potential Melastatin 3 Ion Channel Function in Natural Killer Cells From Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Patients. Front Immunol. 2019 Oct 31;10:2545. doi: 10.3389/fimmu.2019.02545. PMID: 31736966; PMCID: PMC6834647.
Toljan K, Vrooman B. Low-Dose Naltrexone (LDN)—Review of Therapeutic Utilization. Medical Sciences. 2018; 6(4):82. https://doi.org/10.3390/medsci6040082
Parkitny L, Younger J. Reduced Pro-Inflammatory Cytokines after Eight Weeks of Low-Dose Naltrexone for Fibromyalgia. Biomedicines. 2017 Apr 18;5(2):16. doi: 10.3390/biomedicines5020016. PMID: 28536359; PMCID: PMC5489802.
Oaklander, Anne Louise , Alexander J. Mills, Mary Kelley, Lisa S. Toran, Bryan Smith, Marinos C. Dalakas, Avindra Nath, Peripheral Neuropathy Evaluations of Patients With Prolonged Long COVID, Neurol Neuroimmunol Neuroinflamm May 2022, 9 (3) e1146; DOI: 10.1212/NXI.0000000000001146
Xie, Y., Xu, E., Bowe, B. et al. Long-term cardiovascular outcomes of COVID-19. Nat Med 28, 583–590 (2022). https://doi.org/10.1038/s41591-022-01689-3
Liu, Luke D., Deborah L. Duricka, Stellate ganglion block reduces symptoms of Long COVID: A case series, Journal of Neuroimmunology, Volume 362, 2022, https://doi.org/10.1016/j.jneuroim.2021.577784
Taub PR, Zadourian A, Lo HC, Ormiston CK, Golshan S, Hsu JC. Randomized Trial of Ivabradine in Patients With Hyperadrenergic Postural Orthostatic Tachycardia Syndrome. J Am Coll Cardiol. 2021 Feb 23;77(7):861-871. doi: 10.1016/j.jacc.2020.12.029. PMID: 33602468.
Castro-Marrero J, Segundo MJ, Lacasa M, Martinez-Martinez A, Sentañes RS, Alegre-Martin J. Effect of Dietary Coenzyme Q10 Plus NADH Supplementation on Fatigue Perception and Health-Related Quality of Life in Individuals with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: A Prospective, Randomized, Double-Blind, Placebo-Controlled Trial. Nutrients. 2021 Jul 30;13(8):2658. doi: 10.3390/nu13082658. PMID: 34444817; PMCID: PMC8399248.
Blackett JW, Li J, Jodorkovsky D, Freedberg DE. Prevalence and risk factors for gastrointestinal symptoms after recovery from COVID-19. Neurogastroenterol Motil. 2022 Mar;34(3):e14251. doi: 10.1111/nmo.14251. Epub 2021 Sep 1. PMID: 34468069; PMCID: PMC8646904.
Aldous, Thomas R, J, Forsyth R, Chater A, Williams M (2021) The Influence of a blend of Probiotic Lactobacillus and Prebiotic Inulin on the Duration and Severity of Symptoms among Individuals with Covid-19. Infect Dis Diag Treat 5: 182. DOI: 10.29011/2577-1515.100182
Addison AB, Wong B, Ahmed T, Macchi A, Konstantinidis I, Huart C, Frasnelli J, Fjaeldstad AW, Ramakrishnan VR, Rombaux P, Whitcroft KL, Holbrook EH, Poletti SC, Hsieh JW, Landis BN, Boardman J, Welge-Lüssen A, Maru D, Hummel T, Philpott CM. Clinical Olfactory Working Group consensus statement on the treatment of postinfectious olfactory dysfunction. J Allergy Clin Immunol. 2021 May;147(5):1704-1719. doi: 10.1016/j.jaci.2020.12.641. Epub 2021 Jan 13. PMID: 33453291.
Yan CH, Mundy DC, Patel ZM. The use of platelet-rich plasma in treatment of olfactory dysfunction: A pilot study. Laryngoscope Investig Otolaryngol. 2020 Feb 21;5(2):187-193. doi: 10.1002/lio2.357. PMID: 32337347; PMCID: PMC7178450.
Article last updated August 2022. Check the Long Covid News page to see if there’s new info.